[ad_1]
Understanding Suboxone and its Rold in Opiate and Opioid Addiction Treatment
Suboxone is an opioid prescription drug which is used to treat opioid and opiate dependency. Opioid and opiate are frequently used interchangeably, however there is a difference between the two. Opioid is the word to describe any fully synthetic drugs which work similar to their natural counterparts, such as Fentanyl and Vicodin. Opiates are derived from plants, mainly the Poppy plant which produces opium, and make up substances such as Heroin and Morphine. As stated, prior Suboxone is an opioid prescription drug, this shows that Suboxone is a fully synthetic substance. Suboxone consists of a combination of two drugs which are Buprenorphine, which is a partial opioid agonist, and Naloxone, which is a full opioid antagonist.
Each of the main two active substances of Suboxone play a role in how Suboxone treats opioid/opiate addiction. Buprenorphine assists in reducing cravings for opioids/opiates as well as assists with either dampening or removing withdrawal symptoms. While on Buprenorphine a person should notice a more regulated brain chemistry being free of other substances. The Naloxone part of the medication plays an equal role in the treatment of opiate addiction. Naloxone blocks the pleasurable effects of opioids and opiates in the brain which assist in decreasing dependency. Naloxone also will cause the individual to go into a mild state of withdrawal in the event of a relapse, which deters the individual from continued relapse(s).
There are many benefits to starting treatment with Suboxone. The largest benefit is if used correctly Suboxone will successfully assist a person addicted to opioids and/or opiates in a healthy and pain-free method towards a life of sobriety. The Naloxone in Suboxone is of great benefit as it deters an individual from having a relapse no matter how small while keeping them in a sustained state of sobriety. The Buprenorphine in Suboxone is of benefit as it will keep the person in addiction treatment from experiencing withdrawal symptoms while they work on other important areas of their recovery. One of the only drawbacks to Suboxone is there can be some unpleasant side effects with this medication. Some of these side effects may include headaches, dizziness, tongue pain, nausea, increased sweating, blurred vision, vomiting, insomnia, constipation, or drowsiness. As these symptoms may be unpleasant, they are greatly better than continued substance abuse which often leads to overdose and potentially death. There are many over-the-counter comfort medications which can assist in treating and alleviating the possible side effects of taking Suboxone.
Risks and Dangers Associated with Using Opiates After Suboxone
There are times when some individuals that have completed an addiction treatment program such as one with Suboxone, believe that they are able to use in a controlled or recreational manner. This is almost never true, and that usage will have many risks and dangers associated with this mindset. The most dangerous of all of these is the potential for overdose. As with any substance usage whether opiates/opioids or any other substance the chance of overdose is always a possibility. There are many factors which go into what can cause an overdose after or during treatment that many people are unaware of and often lead to fatal overdoses. First, which is more commonly known, is that as a person has any length of sobriety, their tolerance for that substance decreases. Often individuals will want to use the same amount of a substance that they once were used to, but with the decreased tolerance those elevated levels of the substance can easily be beyond a fatal level.
Another not as commonly thought of area with overdoses is the ever-increasing amount of chemically altered substances. It is highly common that many of the most abused opiates such as heroin and opioids such as Vicodin are chemically altered by the addition of Fentanyl. Many current prescription drugs sold on the street, such as Vicodin, are just Fentanyl and fillers pressed into the form of the prescription pill. Fentanyl is considerably stronger than the intended substance and if the amount is higher, it can easily lead to overdose and often fatal overdoses. Another new substance that is being commonly mixed with opiate and opioids as well as many other substances is Xylazine. This drug is used for veterinary sedation and is not an opioid. The danger with this drug being chemically mixed into opioids or opiates is that unlike an opioid being mixed in, Xylazine is not reactive to Naloxone. These are just some of the drugs that are being combined to increase potency and new and stronger variations and substances are coming out at alarming rates.
There is a concept called state dependent learning which can play a role in overdoses, both fatal and non-fatal. State dependent learning is a phenomenon in which a person remembers information if their mental or physical state is the same at the time of learning or encoding the information as the time of recall. How this has been seen to have negative affects is common with substance usage. A person will learn how to interact in certain environments, or more specially locations, while they are intoxicated with a substance. Often those that abuse a substance have frequent places where this happens, which causes a form of state dependent learning. After sobriety often those places and environments are not available to the person anymore. This causes a person, if a relapse is to happen, to have to use the substance in new environments. Which in turn causes the drug to appear to have a greater affect on the person, which can assist in leading to an overdose.
Full relapse is a risk of any opioid or opiate use after completing treatment. Just one usage is enough to cause a person to go fully into relapse and back into the throws of full active addiction. And this usage which can cause a relapse can be from either recreational usage or from prescribed usage. It is important that even if being prescribed an opioid for a legitimate reason to let your physician know of your history so it can be monitored or alternative pain management can be attempted. As well as you should let your physician know it is important that you have other social support resources on hand in the event of any thoughts of relapse.
Recommendations for Opioid or Opiate Usage After Suboxone Treatment
If an opiate or opioid is absolutely medically required, it is very important to be open and honest with your physician about your past substance history. There are often other medications outside of opiates and opioids which can be used pending the situation and any alternative means should be attempted first. There is a wealth of alternative pain management options available, all pending what your aliments are. An example would be to increase exercise for stabilizing muscle groups or physical therapy, to relieve some physical symptoms of muscular pain. Also, for pain management Suboxone itself can be commonly used. As previously mentioned, the Naloxone aspect with Suboxone is ideal to assist in decreasing the chances for another relapse. If an opioid is required and medically necessary, there are things you can do to watch out for signs of relapse.
A main thing you should watch out for is the dosage and frequency of any opioid or opiate medication you are taking. First and foremost, you should only take medication as prescribed by your physician. Regarding your medication it is extremely important for you to journal the dosage and the frequency of the medication you are taking. If you notice any increases or inconsistencies, such as holding off on what prescribed dosage to double another, this is signs of a potential relapse. Report any changes to dosage and/or frequency to your physician.
Implementing harm reduction strategies are another way to assist if opioid or opiate use is required after addiction treatment. Harm reduction strategies include a variety of measures put in place to assist with any behavior that has a high level of risk involved. A good example of this would be the use of seat belts. Even though no one plans to wreck their car, wrecks do happen. The use of a seat belt every time you are in a vehicle is a way to diminish the chance of harm in the event something goes wrong with that trip in your automobile. Harm reduction works the same way with opioid or opiate usage. If it is needed to use an opioid after addiction treatment you can place in safeguards to help reduce the harm. One would be to have someone else have control over your medication and only give you the prescribed dosage at that time, which would eliminate the ability for you to be able to abuse the medication. Alerting your sponsor would be important as they would understand the chance for urges and relapse in the situation and be there for you as a support. And you can do this with all the support structures you have.
Additional Resources and Support for Patients in Addiction Recovery
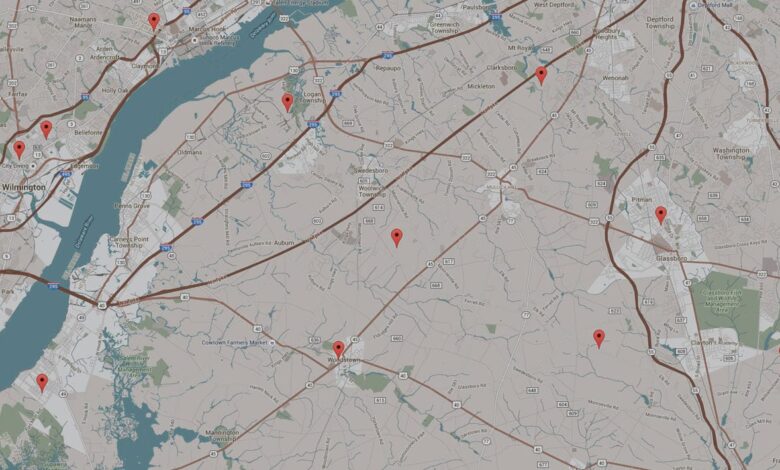
To assist with continued recovery after completion of a treatment program such as with the usage of Suboxone there are many options to help. One of the most common is the usage of support groups or peer recovery programs. The most commonly used support group is Narcotics Anonymous (N.A.) and has been highly successful for many in recovery. Sometimes individuals may have a problem with the higher power concept in Narcotics Anonymous, if this is the case for you there is NA Agnostica and Secular NA. Some also may attend Alcoholics Anonymous (A.A.) to get some support as well. For the Peer Recovery Programs, those vary greatly depending on the area that you live in. The basic concept here is that there are programs in which others that have successfully completed a treatment program and are in active recovery assist one another, especially those in need. A good starting point to find which of these programs are available in your area would be to contact your local Drug and Alcohol Commission or search on SAMHSA (Substance Abuse and Mental Health Services Administration) website.
It is highly important to have a comprehensive relapse prevention plan. This should have been completed with your therapist or case worker during any in-patient or intensive out-patient treatment. If this did not happen, do not worry, as you can still create one. The main part of a relapse prevention plan is to help you recognize your own behaviors that may lead to a relapse. There are three main factors here that can lead to relapse which are emotional, physical, and mental. In each of these areas you need to acknowledge any warning signs that will assist in providing insight that a relapse is starting up. Relapses often start well before the actual substance is used, it is other areas of life that bring up these feelings to want to use. It is identifying these scenarios and knowing how to stop them before substance usage happens.
The second part of a relapse prevention plan is knowing what to do if you do fully relapse or come close. One of the first parts should be preventive measures such as attending a support meeting, exercising, therapy, or journaling. Next part is to have an outlined plan in the event preventative measures do not work. This would include knowing who to contact to assist you with re-entering a treatment program. If you are sponsoring others in a support group, you would need to assist them with getting a new sponsor for the time, as well as letting your sponsor know. Let your social supports know of the relapse and how to assist you into getting back to a point of recovery. It is important to understand that often relapses happen and many pull through them and get right back to a life of recovery.
There are many other possibly resources and support that you can also incorporate into your recovery. One resource is the use of online communities, which would be similar to that of other support groups. There are holistic treatment options available to assist in continued recovery, one of the most common being Cognitive Behavioral Therapy. Other very useful holistic treatment options are stress management, life skills lessons, strengthening interpersonal skills, and increasing your overall health and wellbeing via adding exercise and a better diet. All of these are useful to any individual, not just someone in addiction recovery, and can assist with an improved quality of life as well as serve as an additional support to a continued life of sobriety.
[ad_2]
Source link




